Ciprofloxacin Resistance in Escherichia Coli Strains Isolated from Urinary Tract Infections
DOI:
https://doi.org/10.59675/P321Keywords:
Escherichia coli, urinary tract infection, ciprofloxacin, antibioticAbstract
Background: The purpose of this investigation was to show how resistant E. Coli is towards the fluoroquinolone treatment Ciprofloxacin. There were 140 specimens in total. It is widely recognized that infections of the urinary tract are a prevalent condition in women and men and different ages. The bacteria that cause E. Coli becomes more resistant as a result of increased consumption of antibiotics, which means this symptom is dangerous on a worldwide scale.
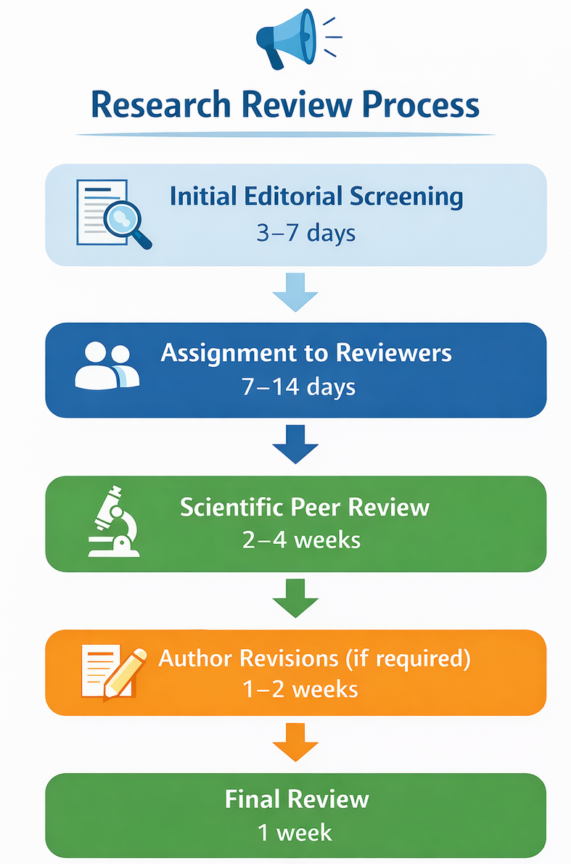
Methods: Within Al-Hindya Teaching Hospital, specimens of urine involving individuals of different age have been employed to isolate the E. Coli germs. The required separation procedures have been conducted, comprising genetic sequencing of the bacterial strain carbon monoxide gene, microscopical examination, plus biochemical examinations. The resulting isolates were subjected to the procedure called polymerase chain reaction (PCR), and their resistance to antibiotics was assessed by putting discs containing antibiotics on the Mueller_ Hinton agar.
Results: Compared to males, girls had a greater rate of E. Coli disease. The bacteria that underwent responsiveness testing employed ciprofloxacin, and that microbes rate of resistance to this antibiotic was somewhat higher than its level of sensitivity. Investigating the growing resistance of Ur pathogenic E. Coli bacterium to the antibiotic ciprofloxacin is the goal objective this investigation.
References
- Mwakyoma AA, Kidenya BR, Minja CA, Mushi MF, Sandeman A, Sabiti W, Holden MT, Mshana SE. Allele distribution and phenotypic resistance to ciprofloxacin and gentamicin among extended-spectrum β-lactamase-producing Escherichia coli isolated from the urine, stool, animals, and environments of patients with presumptive urinary tract infection in Tanzania. Frontiers in Antibiotics. 2023 Jun 5; 2:1164016. DOI: https://doi.org/10.3389/frabi.2023.1164016
- Afsharikhah S, Ghanbarpour R, Mohseni P, Adib N, Bagheri M, Jajarmi M. High prevalence of β-lactam and fluoroquinolone resistance in various phylotypes of Escherichia coli isolates from urinary tract infections in Jiroft city, Iran. BMC microbiology. 2023 Apr 22;23(1):114. DOI: https://doi.org/10.1186/s12866-023-02860-7
- Rippere-Lampe KE, O'Brien AD, Conran R, Lockman HA. Mutation of the gene encoding cytotoxic necrotizing factor type 1 (cnf 1) attenuates the virulence of uropathogenic Escherichia coli. Infection and immunity. 2001 Jun 1;69(6):3954-64. DOI: https://doi.org/10.1128/IAI.69.6.3954-3964.2001
- Moniri R, Khorshidi A, Akbari H. Emergence of multidrug resistant strains of Escherichia coli isolated from urinary tract infections. Iranian Journal of Public Health. 2003;32(4):42-6.
- Arslan H, Azap ÖK, Ergönül Ö, Timurkaynak F. Risk factors for ciprofloxacin resistance among Escherichia coli strains isolated from community-acquired urinary tract infections in Turkey. Journal of Antimicrobial Chemotherapy. 2005 Nov 1;56(5):914-8. DOI: https://doi.org/10.1093/jac/dki344
- Abbott IJ, van Gorp E, Cottingham H, Macesic N, Wallis SC, Roberts JA, Meletiadis J, Peleg AY. Oral ciprofloxacin activity against ceftriaxone-resistant Escherichia coli in an in vitro bladder infection model. Journal of Antimicrobial Chemotherapy. 2023 Feb 1;78(2):397-410. DOI: https://doi.org/10.1093/jac/dkac402
- Akram M, Shahid M, Khan AU. Etiology and antibiotic resistance patterns of community-acquired urinary tract infections in JNMC Hospital Aligarh, India. Annals of clinical microbiology and antimicrobials. 2007 Jan; 6:1-7. DOI: https://doi.org/10.1186/1476-0711-6-4
- Jakobsen L, Lundberg CV, Frimodt-Møller N. Ciprofloxacin pharmacokinetics/pharmacodynamics against susceptible and low-level resistant Escherichia coli isolates in an experimental ascending urinary tract infection model in mice. Antimicrobial Agents and Chemotherapy. 2020 Dec 16;65(1):10-128. DOI: https://doi.org/10.1128/AAC.01804-20
- Nakhjavani FA, Mirsalehian A, Hamidian M, Kazemi B, Mirafshar M, Jabalameli F. Antimicrobial susceptibility testing for Escherichia coli strains to fluoroquinolones, in urinary tract infections. Iranian journal of public health. 2007;36(1):89-92.
- Neyestani Z, Khademi F, Teimourpour R, Amani M, Arzanlou M. Prevalence and mechanisms of ciprofloxacin resistance in Escherichia coli isolated from hospitalized patients, healthy carriers, and wastewaters in Iran. BMC microbiology. 2023 Jul 17;23(1):191. DOI: https://doi.org/10.1186/s12866-023-02940-8
- Ayobola ED, Oscar WO, Ejovwokoghene EF. Plasmid-mediated quinolone resistance genes transfer among enteric bacteria isolated from human and animal sources. AIMS microbiology. 2021 Jun 9;7(2):200. DOI: https://doi.org/10.3934/microbiol.2021013
- Mandal J, Acharya NS, Buddhapriya D, Parija SC. Antibiotic resistance pattern among common bacterial uropathogens with a special reference to ciprofloxacin resistant Escherichia coli. Indian Journal of Medical Research. 2012 Nov 1;136(5):842-9.
- Holt JG, Krieg NR, Sneath PH, Staley JT, Williams ST. Bergey’s Manual of Determinative bacteriology, 9thedn. Williams and Wilkins, Baltimore, USA. 1994:749-55.
- JF M. Biochemical tests for identification of medical bacteria. Lippinccot, Williams & Williams, Baltimore. 2000.
- Mackie TJ. Practical medical microbiology. Churchill livingstone; 1996.
- Al-Ghanimi AA, Al-Zughaibi AS. Molecular Identification of Acinetobacter baumannii and Staphylococcus aureus isolated from wound infections in Karbala governorate Iraq. InAIP Conference Proceedings 2022 Dec 2 (Vol. 2547, No. 1). AIP Publishing. DOI: https://doi.org/10.1063/5.0113631
- Mehdipour S, Doosti A, Ghasemi Dehkordi P. Detection of cytolethal distending toxin (cdt) and cytotoxic necrotizing factor (cnf) genes among Escherichia coli isolates from Iranian sheep carcasses. Comparative clinical pathology. 2012 Dec; 21:1683-8. DOI: https://doi.org/10.1007/s00580-011-1349-6
- Perez-Roth E, Claverie-Martın F, Villar J, Mendez-Alvarez S. Multiplex PCR for simultaneous identification of Staphylococcus aureus and detection of methicillin and mupirocin resistance. Journal of clinical microbiology. 2001 Nov 1;39(11):4037-41. DOI: https://doi.org/10.1128/JCM.39.11.4037-4041.2001
- Jonas D, Speck M, Daschner FD, Grundmann H. Rapid PCR-based identification of methicillin-resistant Staphylococcus aureus from screening swabs. Journal of Clinical Microbiology. 2002 May;40(5):1821-3. DOI: https://doi.org/10.1128/JCM.40.5.1821-1823.2002
- Bauer AW, Kirby M, Sheris JD, Turch M. Antibiotic resistance testing by standard single disc method. Am J Clin Pathol. 1966;45(4):493-6. DOI: https://doi.org/10.1093/ajcp/45.4_ts.493
- Thong KL, Lai MY, Teh CS, Chua KH. Simultaneous detection of methicillin-resistant Staphylococcus aureus, Acinetobacter baumannii, Escherichia coli, Klebsiella pneumoniae and Pseudomonas aeruginosa by multiplex PCR.
- Wang S, Zhao S, Zhou Y, Jin S, Ye T, Pan X. Antibiotic resistance spectrum of E. Coli strains from different samples and age-grouped patients: a 10-year retrospective study. BMJ open. 2023 Apr 1;13(4): e067490. DOI: https://doi.org/10.1136/bmjopen-2022-067490
- Gobernado M, Valdés L, Alós JI, Garcia-Rey C, Dal-Ré R, García-de-Lomas J, Spanish Surveillance Group for E. Coli Urinary Pathogens. Quinolone resistance in female outpatient urinary tract isolates of Escherichia coli: age-related differences. Rev Esp Quimioter. 2007 Jun 1;20(2):206-10.
- Nakhjavani FA, Mirsalehian A, Hamidian M, Kazemi B, Mirafshar M, Jabalameli F. Antimicrobial susceptibility testing for Escherichia coli strains to fluoroquinolones, in urinary tract infections. Iranian journal of public health. 2007;36(1):89-92.
- Moniri R, Khorshidi A, Akbari H. Emergence of multidrug resistant strains of Escherichia coli isolated from urinary tract infections. Iranian Journal of Public Health. 2003;32(4):42-6.
- Czajkowski K, Broś-Konopielko M, Teliga-Czajkowska J. Urinary tract infection in women. Menopause Review/Przegląd Menopauzalny. 2021 Apr 21;20(1):40-7. DOI: https://doi.org/10.5114/pm.2021.105382
- Griebling TL. Urinary tract infection in women. Urologic diseases in America. 2007; 7:587-619. DOI: https://doi.org/10.5005/jp/books/10673_105
- Bashir MF, Qazi JI, Ahmad N, Riaz S. Diversity of urinary tract pathogens and drug-resistant isolates of Escherichia coli in different age and gender groups of Pakistanis. Tropical journal of pharmaceutical research. 2008 Sep 11;7(3):1025-31. DOI: https://doi.org/10.4314/tjpr.v7i3.14687
- McGregor JC, Elman MR, Bearden DT, Smith DH. Sex-and age-specific trends in antibiotic resistance patterns of Escherichia coli urinary isolates from outpatients. BMC family practice. 2013 Dec; 14:1-5. DOI: https://doi.org/10.1186/1471-2296-14-25
- Bennett CJ, Young MN, Darrington H. Differences in urinary tract infections in male and female spinal cord injury patients on intermittent catheterization. Spinal Cord. 1995 Feb;33(2):69-72. DOI: https://doi.org/10.1038/sc.1995.17
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Academic International Journal of Pure Science

This work is licensed under a Creative Commons Attribution 4.0 International License.